Breast cancer is usually talked about as a disease affecting women, but men have breast tissue, too, and they can develop breast cancer. Knowing the basics helps you spot changes early and act fast.
What is Breast Cancer in Men?
Breast cancer is the uncontrolled growth of abnormal cells in breast tissue. Men have a small amount of breast tissue (mostly behind the nipple), and the same main types seen in women can occur in men:
- Invasive ductal carcinoma (IDC)
- Invasive lobular carcinoma (ILC)
- Ductal carcinoma in situ (DCIS)
These types behave in men much like they do in women.
How Common is It?
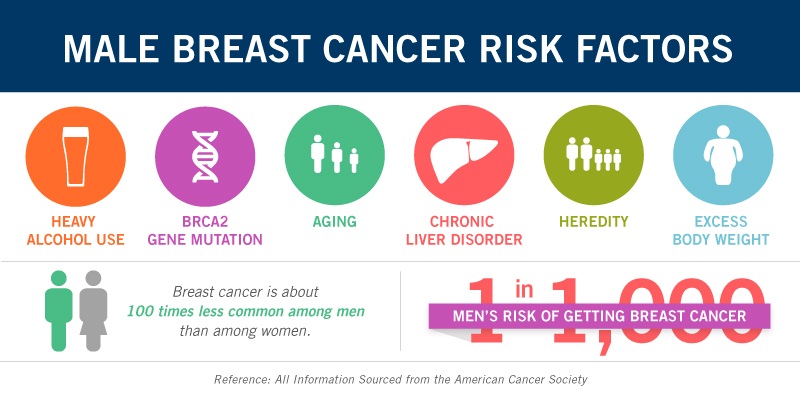
Male breast cancer is uncommon. The CDC estimates that about 1 out of every 100 breast cancers diagnosed in the U.S. is found in a man.
For 2025, the American Cancer Society projects about 2,800 new cases of invasive breast cancer in men and about 510 deaths in men. The average lifetime risk for a U.S. man is about 1 in 726.
ACS also notes that breast cancer is ~100× less common among white men than white women and ~70× less common among Black men than Black women, and that Black men with breast cancer tend to have a worse outlook—important disparities that underscore the need for awareness and timely care.
Signs and Symptoms to Watch for
Contact a healthcare provider if you notice any of the following on one side or both:
- A lump or swelling in the breast or underarm
- Nipple discharge
- Redness, scaling, or flaky skin on the breast or nipple
- Irritation, dimpling, or puckering of breast skin
- Nipple turning inward (retraction) or nipple pain
Sometimes cancer spreads to lymph nodes near the collarbone or under the arm and causes a lump before a breast lump is felt. These symptoms can also be caused by conditions that aren’t cancer, but they should always be checked.
Who is at Higher Risk?
Your risk may be higher if you:
- Have a strong family history of breast cancer or carry BRCA1/BRCA2 gene changes (especially BRCA2)
- Have had chest radiation
- Have conditions that raise estrogen levels (e.g., Klinefelter syndrome, certain liver diseases)
- Have obesity or certain testicular conditions
Risk increases with age. Talk to your clinician about whether genetic counseling/testing is right for you.
How is it Treated?
Treatment depends on the tumor’s size and whether it has spread. Options can include surgery, chemotherapy, radiation, hormone therapy, and targeted therapy—similar to treatments used for women. Your care team will tailor a plan to you.
Bottom Line
Breast cancer in men is rare, but real. If you notice a new lump, nipple changes, skin dimpling, or discharge, don’t wait—see your healthcare provider right away. Early evaluation leads to better outcomes.



